How is colon cancer different from rectal cancer?
Colon cancer and rectal cancer are often referred to as colorectal cancer, but there are differences between them. Gastroenterologist Anjani Jammula, MD, explained how colon cancer is different from rectal cancer and how these differences can impact your treatment and recovery.
Some colon facts
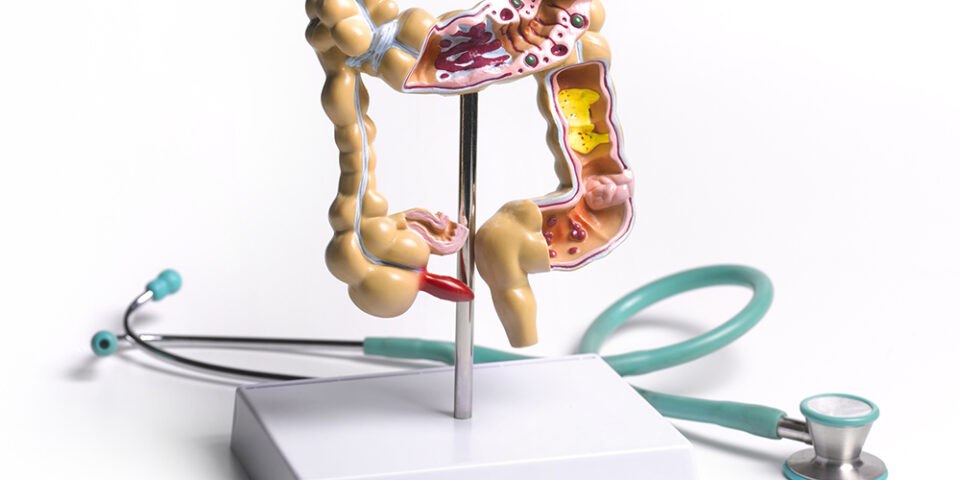
The colon (large intestine) is a muscular tube of about 5 feet in length, and its main function is water absorption. The colon starts at the junction between your small intestine and the large intestine.
There are four parts of the colon: the ascending colon (the section going up), transverse colon (the middle of the colon), descending colon (the section coming down) and sigmoid colon (an S-shaped section).
The last part is called the rectum, which is connected to the body’s exterior through the anus. The job of the rectum is to wait until a certain amount of waste material comes into it and then send nerve signals to your brain that you need to use the bathroom.
How is colon cancer different from rectal cancer?
Cancer can start anywhere in the colon or rectum.
“You can call it colon cancer if it’s not coming from the rectum, just to differentiate the site of origin,” Dr. Jammula said. “For practical purposes, we group them together since they both have common features, but there are differences.”
The common features are:
- Risk factors
- Symptoms
- The number of cancers diagnosed every year
- The genetic makeup of the cancer
Differences include:
For both colon and rectal cancer, early diagnosis is key, so it’s important to be screened and to be aware of any signs or symptoms.
- Colon cancer is equally common in both genders, but rectal cancer is more common in men.
- Radiation is not usually used as a treatment for colon cancer, but it is for rectal cancer.
- Surgery is typically used to treat colon cancer and is a relatively easy procedure, but rectal cancer usually requires chemotherapy and radiation first and can be more difficult to cure.
- Rectal cancer metastasizes easier, spreading beyond the colon.
What are the warning signs of colon and rectal cancer?
Symptoms can be subtle, for example, any change in your bowel habits.
“Some people are like a clock,” Dr. Jammula said. “They drink their cup of coffee in the morning and then four minutes later they’re in the bathroom. For that person, if he’s struggling to have a bowel movement, and he’s not moving his bowels at least once every two or three days, that’s a change for him and it should raise an alarm.”
Same thing with diarrhea or if there is a significant change in the size of the stool.
“Sometimes the diameter of the stool becomes pencil-thin,” she explained. “The reason that happens is because the tumor constricts and decreases the size of the colonic lumen so your stool gets compressed, and by the time it’s exited, the stool is smaller.”
Bleeding is another warning sign.
“There is rectal bleeding and there is blood in the stool,” Dr. Jammula said. “Nine out of 10 times it’s caused by hemorrhoids, but we cannot ignore it because a large colon polyp or cancer in the rectum can also present in such a way. So, regardless of the person’s age, if someone is complaining of blood in the stool, especially if it’s a new symptom for them, I will offer them a colonoscopy to assess the cause.”
Other symptoms include new onset abdominal pain, feeling fatigued or weak, unexplained weight loss, and rectal tenesmus, which is the feeling of needing to have a bowel movement that’s not relieved by having one.
“The reason rectal tenesmus happens is because the nerve endings in the rectum are very sensitive,” Dr. Jammula said. “It can be an inflammation, it can be a polyp, or it can be cancer, and when that gets irritated, patients have that sensation.”
If you are noticing any of these warning signs, don’t wait. Reach out to your doctor. Colon cancer is treatable and beatable. It can also be prevented through regular screening.
When is it appropriate to be screening for colorectal cancer?
It depends on your risk. For people with average risk, colorectal cancer screening should begin at age 45. For those who are at high risk, such as people with a family history of colorectal cancer, screening should begin at age 40 or 10 years younger than the youngest family member with cancer, whichever is the earliest.
“Your family history certainly matters,” Dr. Jammala said. “Your first degree relatives – a parent or a sibling – definitely put you at a much higher risk than a second or third degree relative.”
If you have inflammatory bowel disease or ulcerative colitis patients, screening should begin eight years after the diagnosis and be repeated every one to two years.
If someone has had any type of cancer, screening for colorectal cancer should begin as early as their 20s.
Talk to your doctor about your risk to make sure you’re on top of your colorectal health.
Find a doctor
Whether you’re looking for a primary care physician or need to see a specialist, we’re here to help with experienced, compassionate care near you.
Find a Doctor