How to know if you have hemophilia
Hemophilia is an inherited disorder in which the blood doesn’t clot properly. Stephanie Ambrose, DO, and Leslie Gilbert, MD, explain who’s at risk for hemophilia, how it’s diagnosed, how it’s treated, and more.
Transcript
Caitlin Whyte (Host): Knowing if you have a medical condition is something that many of us have tried to figure out on our own. So, we’re going to help you out and give you some tips on how to know if you have hemophilia today. We are joined by two of our very own experts, Dr. Stephanie Ambrose, the Medical Director of the South Carolina Hemophilia Treatment Center, and Dr. Leslie Gilbert, Director at the South Carolina Hemophilia Treatment Center Upstate.
This is Flourish. A podcast brought to you by Prisma Health. I’m Caitlin Whyte. So, Dr. Ambrose, I’ll start with you today. What is hemophilia and what causes it?
Stephanie Ambrose, DO (Guest 2): So hemophilia is usually an inherited disorder in which the blood doesn’t clot properly. It’s generally an X-linked disorder, meaning that it’s passed from a mother who is a carrier of hemophilia. And if she passes that affected X chromosome onto a daughter, the daughter will also be a carrier like mom, of hemophilia.
However, if mom passes on the affected X chromosome to a son, he will actually be affected with hemophilia because he only has one X chromosome. A diagnosis of hemophilia means that a person is missing the ability to produce an essential blood clotting factor normally. Usually this clotting factor is going to either be factor eight in patients who have hemophilia A, or factor nine in patients who have hemophilia B. In mild or moderate hemophilia, the clotting factor is produced, but it’s at a grossly reduced amount. And then in patients who have severe hemophilia, the clotting factor is actually not produced at all.
Host: Gotcha. So Dr. Gilbert, who would you say is at risk for hemophilia?
Leslie Gilbert, MD (Guest 1): So as Dr. Ambrose said, it’s mostly going to affect males because it’s X-linked. And about two thirds are going to have a family history, meaning mom had a mutated X chromosome and passed it onto a son. If mom has a mutated X chromosome, it’s about a 50-50 chance that she passes it to a son. But we also know that one third of patients don’t have a family history, it’s a new mutation in that patient. So sometimes it’s a surprise. So again, mostly in males, but we do know that there are occasional though rare, female carriers, meaning they have one normal X chromosome, one abnormal X chromosome and for some reason they express that abnormal X chromosome more. And they also can have low factor levels and be classified as hemophilia.
Host: Okay. Thank you. Well, let’s talk about some signs or symptoms, Dr. Ambrose. What are some things we can look out for talking about hemophilia here?
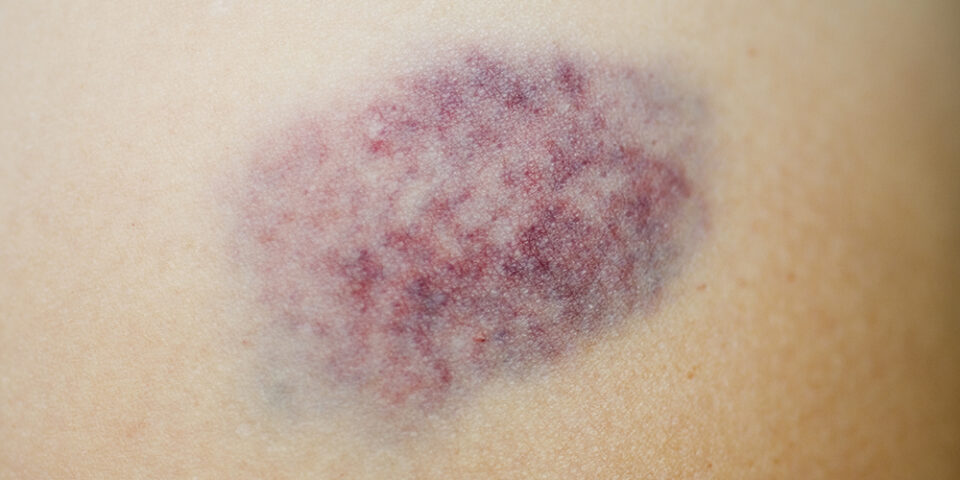
Guest 2: So signs of hemophilia are really going to be increased bleeding and bruising symptoms. So patients with hemophilia bleed more because they’re missing that essential clotting factor that we were talking about, again, usually either factor eight or factor nine. And they’re at increased risk really, of all types of bleeding. But in particular, we really find that these patients are at increased risk of bleeding into their joints and muscles.
Host: And Dr. Gilbert, let’s talk about timing. When is hemophilia typically diagnosed?
Guest 1: So it depends on the severity of hemophilia. So, you have severe hemophilia and those patients don’t make any of the either factor eight or factor nine that help them clot, moderate hemophilia when they make about one to 5% and then mild where they make five to 40%. Normal is 40 to 50% or higher. So depending on the severity, they may present earlier. Now someone with a family history, we know they’re going to be at risk. We’re going to check them in the newborn nursery, and figure out if they have hemophilia shortly after birth. Males with hemophilia that is severe, even outside of family history, are typically going to present an infancy, usually from heel sticks for lab draws in the newborn nursery, or circumcision that bleeds and doesn’t heal correctly. But most all, are going to present sometime in infancy or for the mild cases, early childhood.
Host: Well, let’s talk about some treatment options now. Dr. Ambrose, what does the treatment process look like and can hemophilia be cured?
Guest 2: So currently the gold standard for treating hemophilia is to replace the missing clotting factor so that the blood can then clot properly. So for example, if a patient has hemophilia A and they’re missing factor nine, and they have a bleeding event, then we would treat them with a factor 8 product, meaning that we’re going to give them factor eight back, to increase their factor eight levels and to stop the bleeding. There are several newer medications that are on the market to treat certain types of hemophilia, but the goal of every one of those treatment options is really, in some way or another to help form a stable clot and to stop the bleeding.
Presently there is no known cure for hemophilia. There is a newer liver directed gene therapy product that was recently approved for patients with hemophilia B, in November of 2022. However, this therapy is not considered a cure. We know that over time that those patients will likely lose the expression of the factor nine that they make, and can possibly fall back into the ranges of hemophilia.
We are hopeful though. There are gene editing therapy trials that are ongoing and we’re hopeful, um, for a potential cure in the future, but we’re not quite there yet.
Host: Gotcha. All right. Well, Dr. Gilbert, can someone with hemophilia live like a typical or quote unquote normal life? Can they do sports? What does life with hemophilia look like?
Guest 1: With some of the newer options for treatment over the past couple of decades, our goal is that they can live as normal a life as possible. But to do that, they have to replace their factor regularly to keep from bleeding. So, that for the most part, for most factors is still IV. They have to learn to give themself an IV factor.
There are some newer medications that are shots, subcutaneous shots, but they do have to learn to give themselves some kind of medication at home, whether that’s infusing an IV medication one to three times a week or doing a shot every one or two weeks. But they can play sports safely.
We do recommend no contact sports of course, cause there’s no way we’re gong toi make them safe for contact sports. But I do have patients who play basketball. They play baseball. They just have to learn that they need to give factor beforehand. They are going to be more prone to joint issues and bleeding and but we are able to make it as safe as possible. So can they do things they want to do, yes. But is it completely normal? No. It it, it takes a little extra work and planning.
Host: It’s good to hear that there are lots of options for people living with hemophilia. On this topic. Dr. Ambrose, does hemophilia get any worse with age?
Guest 2: So the diagnosis of hemophilia itself doesn’t worsen with age. However, as mentioned previously, patients with hemophilia are at an increased risk of all types of bleeding, particularly in their joints and in their muscles. So bleeding into a joint can cause breakdown and destruction that is irreparable.
So we really try to prevent this whenever we can. Um, if a patient sustains multiple joint bleeding events in their life, they develop chronic joint disease and arthritis in those joints. This can lead to issues with chronic pain and decreased mobility that worsens with age, and can cause significant decreases in one’s overall quality of life.
This is why our goal for us is to help every patient with hemophilia prevent bleeding whenever possible. In patients at risk for frequent bleeding, we really recommend starting prophylactic treatments like Dr. Gilbert said with either several times a week, um, IV infusions with replacement factor or with some of the newer medications on the market.
We really try to push to start those at an early age to help to prevent some of these bleeding issues, events and complications in patients. So that hopefully we can help preserve their joints as they get older.
Host: All right, well wrapping up here, Dr. Gilbert, are there lifestyle changes that you can make or anything else that you can do to help manage the condition?
Guest 1: Like we said earlier, there’s not a cure, but there are ways to, uh, minimize damage over time. The biggest thing is joint damage over time. So staying active, eating a healthy diet, staying at a healthy weight to minimize the pressure and trauma to the joints, is important for sure.
Guest 2: I also would like to put a plug in for both myself and for Dr. Gilbert. It’s also, very, very recommended, um, that patients with hemophilia get annual comprehensive evaluations at hemophilia treatment centers. These centers are specialized in the care of patients with bleeding disorders.
Currently, Prisma Health has the only federally supported hemophilia treatment centers in the state with locations both in Columbia and Greenville. So it’s really important that over time, that patients place this at a high priority so that they can get the care for their hemophilia that they need, particularly as they age.
Guest 1: I would also say that the hemophilia treatment centers, it’s a bit of a misnomer. We treat all bleeding disorders. So hemophilia is one of the main bleeding disorders we see. But, with March being bleeding disorders awareness month, we treat von Willebrand disease, other factor deficiencies and platelet disorders as well.
Host: Well, these are some great tips. So important to know. Thank you so much, both of you for joining me today.
For more information and other podcasts just like this one, head on over to PrismaHealth.org/Flourish. This has been Flourish, a podcast brought to you by Prisma Health. I’m Caitlin Whyte. Stay well.
Read More